
Program of All-Inclusive Care for the Elderly (PACE) is a fully capitated, fully integrated, and comprehensive care program for adults age 55 or older living with chronic illnesses or disabilities. PACE has become the gold standard of care for the frail elderly. As the name suggests, PACE is an “all-inclusive” model of care, which means PACE organizations are at full risk and required to provide, or plan to provide, all service needs of their participants under a capitated payment system. A complete understanding of the cost structure of PACE and key drivers of fixed and variable costs is critical for PACE organizations to effectively manage risk and optimize financial performance. So what does the cost structure of a PACE program look like and what are the critical cost elements that influence financial performance?
Overview: All-Inclusive Care
PACE has a capitated payment system in which PACE organizations are paid an amount per member per month (PMPM). Funding from multiple sources is combined to meet all participant care needs. This pooled capitation consists of four main funding sources: Medicare Part A and B, Medicare Part D, Medicaid, and private pay (uncommon). In return, PACE organizations are responsible for coordinating and providing comprehensive care to their enrolled participants. This all-inclusive care model includes all services normally covered by Medicare and Medicaid. As the term “all-inclusive” suggests, there are very few exceptions.
Capital Costs/Start-Up Expenses
A significant capital investment is required to develop a PACE program. In most cases, the most significant part of the capital investment is the brick and mortar component, developing a PACE center. A PACE center is the hub of a PACE program’s operation and is a required element of becoming a PACE organization. The cost of the PACE center will vary depending on many factors including the square footage; whether the building will be built, bought, or leased; the condition of the building; and the construction market landscape. This is typically a multimillion-dollar investment.
In addition, developing PACE will require start-up costs during the 12- to 18-month development and implementation period. Start-up expenses consist of salaries and benefits for key staff hired prior to becoming operational; consulting expenses for assistance with navigating the feasibility study and application and development process; and costs associated with getting systems in place, such as an electronic medical record (EMR) and third-party administrator (TPA).
Interdisciplinary Team
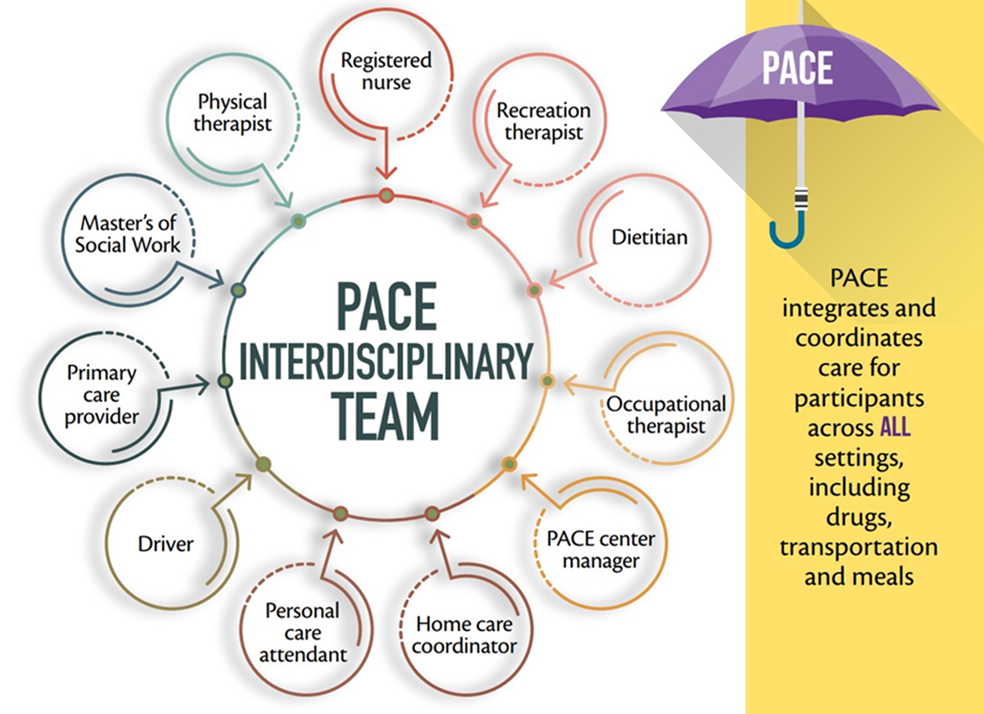
The heart and soul of a PACE program is the PACE interdisciplinary team (IDT). The IDT is responsible for developing a care plan for each participant and coordinating their care needs across all health care settings.
Figure 1: PACE Interdisciplinary Team
 Source: National PACE Association
Source: National PACE Association
The IDT is based in the PACE center and may consist of all employed staff or include contract labor for certain positions. Costs related to the IDT are mainly salaries, benefits, contract labor, and miscellaneous other expenses such as mileage reimbursement and education. IDT members can handle a caseload based on the number of enrolled participants or PACE center attendees that varies based on the individual discipline, making this mainly a variable cost component of PACE. The ability to manage staff ratios as enrollment changes is critical to maintain sufficient levels of care and optimize financial performance. The following are the PACE center–based departments represented on the IDT.
- Transportation: A PACE organization is responsible for providing participants with transportation to and from the PACE center as well as to external medical appointments. Depending on whether transportation is provided internally or by a contracted service, costs will include the purchase or lease and operating cost of vehicles, labor for drivers and coordinators, and transportation software for tracking vehicles and scheduling.
- Nutrition: A dietitian is a key member of the IDT, but a PACE program also provides meals to participants attending the PACE center each day, as well as home-delivered meals.
- Social Services/Pastoral Care: PACE programs employ a team of social workers and many times have a chaplain on staff. Expenses include staff salaries, benefits, and travel-related expenses.
- Therapy: The PACE center includes space and equipment to provide physical and occupational therapy to participants attending each day. Expenses include employed or contracted labor costs and supplies.
- Adult Day Care: PACE participants attend the PACE center for adult day care services including personal care, socialization, meals, and activities. Expenses include salaries and benefits for management and care staff, as well as supplies and other activity-related expenses.
- Home Care: Home care is a community-based service, but it is typically managed and coordinated from the PACE center. Expenses include employed or contracted labor costs for home care aides, scheduling staff and management, supplies, and travel-related expenses.
- Primary Care: The PACE center also includes a primary care clinic where participants can be seen by physicians, nurse practitioners, and registered nurses. Expenses include employed or contracted labor costs for physicians and nurse practitioners, salaries and benefits for the nursing and clinic administrative staff, and clinic supplies.
Provider Network
A PACE organization is a provider of services, but it is also a payor. Services that are not provided by employed staff of the PACE organization are provided by a network of contracted providers developed during program implementation. The network consists of providers of outpatient services, laboratory, physician specialists, pharmacy, durable medical equipment (DME), ambulance, dialysis, and institutional settings such as inpatient hospital care, skilled nursing facilities (SNFs), and long-term care facilities.
Figure 2: PACE Network
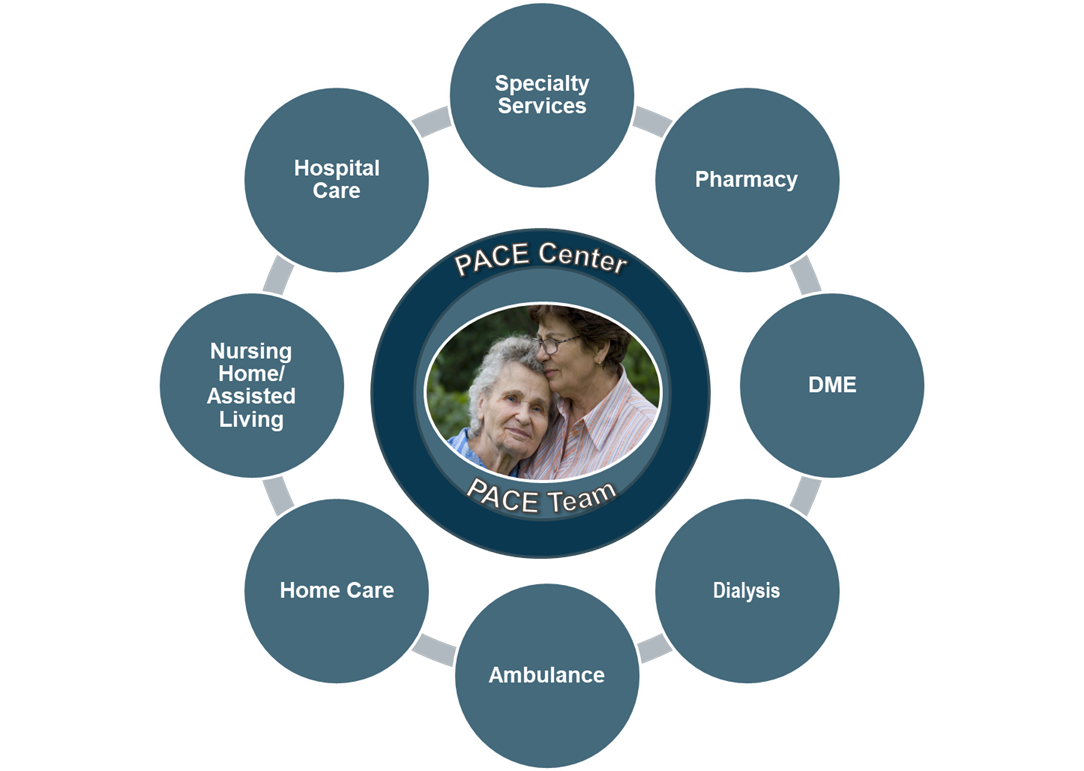 Provider network services are highly variable, typically very costly, and represent the greatest risk for a PACE organization. The critical elements to managing provider network expenses are negotiating fair or favorable contracted rates, effectively managing participant care to avoid high utilization of costly services, and having processes and tools in place to access data and track service utilization and costs in an accurate and timely manner.
Provider network services are highly variable, typically very costly, and represent the greatest risk for a PACE organization. The critical elements to managing provider network expenses are negotiating fair or favorable contracted rates, effectively managing participant care to avoid high utilization of costly services, and having processes and tools in place to access data and track service utilization and costs in an accurate and timely manner.
Pharmacy
One of the more complicated aspects of a PACE program is the pharmacy component. PACE organizations must develop a pharmacy internally or contract with an external pharmacy to provide prescription drugs to PACE participants under the Medicare Part D benefit. Expenses include the cost of drugs and any labor-related costs that depend on whether the pharmacy is developed internally or contracted. In addition, a PACE organization is required to contract with a pharmacy benefit manager (PBM) to administer the claims adjudication and regulatory reporting requirements.
For the most part, the expenses related to operating the pharmacy are reimbursed under the Medicare Part D capitation rate as part of an annual reconciliation process. However, PACE programs are at greater risk for those participants that do not qualify for Medicare benefits.
Administrative/Back Office Support
Administrative and back office support expenses equal about 15 percent of the total expense of a mature PACE program. A majority of this expense is fixed cost, but there is variable cost associated with some non-labor expenses that are driven based on revenue or enrollment.
- Health Information Management: Health information management includes the cost of medical records and coding staff, as well as the cost of an EMR and other contracted consulting services. The non-labor component of this expense is typically variable based on program enrollment.
- Quality/Compliance: Quality and compliance are critical functions of a PACE program to ensure quality outcomes, maintain compliance with state and federal regulations, and generate accurate and reliable data for internal and external reporting purposes. Expenses consist mostly of salaries and benefits for employed staff and are mainly fixed costs.
- Marketing and Intake: The marketing and intake functions are critical to PACE financial success, as these areas drive enrollment growth. One of the most critical factors for successful financial performance is the ability to grow enrollment quickly and achieve a high market penetration rate. Expenses are mainly fixed and consist of salaries and benefits for employed staff and costs for advertising and collateral.
- Claims Processing: As a health plan, PACE organizations are responsible for adjudicating claims submitted for payment by providers that serve PACE participants as part of the PACE provider network. This is another critical function of a PACE program that is either performed internally by the accounting and business office staff or contracted to a TPA. Paying claims in a timely manner helps maintain good relationships with contracted providers, reduces exposure to compliance issues, and improves the integrity of financial statements. In addition, the claims processing function plays a part in improving the accuracy of risk scores that drive Medicare capitation payments.
- Consulting: Consultants play an important role in developing and operating a PACE program. Contracting with a PACE Technical Assistance Center (TAC) to gain an initial understanding of PACE; perform a market and financial feasibility study; navigate the application, development, and implementation process; and provide post-implementation operational support is routine for new PACE organizations. In addition, an actuarial firm is needed to prepare the Medicare Part D bid on an annual basis. Under a normal PACE development scenario, consulting expenses are high in the development period and first year of operations before declining as the program matures.
- Risk Management: Risk management includes the usual property and liability insurance coverage but also includes reinsurance to protect the PACE program against the risk associated with participants that experience an extraordinarily high-cost health care episode or an unusually high accumulation of medical claims that exceed a pre-determined annual cost threshold. A reinsurance policy is very common for PACE organizations, especially in the early years of development.
- Administration: Administration includes the expenses associated with PACE leadership and other administrative expenses, such as association dues, staff education, supplies, postage, and miscellaneous other costs. It also includes overhead and support costs such as finance, accounting, business office, human resources, legal, and information technology expenses. These expenses are commonly provided by a parent company through a corporate allocation or can be directly assigned to the PACE program.
Summary
The most important factors in developing a financially successful PACE program are enrollment growth, market penetration, capitation rates, and expense management. Having a complete understanding of the PACE cost structure will improve the ability of PACE leadership to manage expenses through periods of enrollment volatility and other market pressures, such as a pandemic and workforce challenges.
About Us
As a National PACE Association Technical Assistance Center, Health Dimensions Group (HDG) has successfully assisted many organizations with PACE market and financial feasibility studies, program development and implementation support, and operational improvement. If you would like to learn more about how HDG can assist you in exploring PACE as a solution in today’s challenging health care environment, please contact us at 763.537.5700 or info@hdgi1.com.












