The Program of All-inclusive Care for the Elderly (PACE) centers on the belief that it is better for the well-being of seniors with chronic care needs, and their families, to be served in the community whenever possible. By providing or coordinating all needed medical and supportive services through an interdisciplinary team (IDT), PACE programs are able to provide the entire continuum of care and services to older adults with chronic care needs while enabling them to maintain their independence in their homes for as long as possible. The COVID-19 pandemic has challenged PACE programs from an enrollment and care delivery perspective.
PACE Program Enrollment Impact Due to COVID-19
COVID-19 has had a significant negative impact on census in nearly all areas of senior health care services. Traditional bricks and mortar communities, such as skilled nursing facilities (SNFs), assisted living (AL), and memory care assisted living (MCAL) have experienced a significant decline not only in census, but also in referrals and future pipeline activity. Other post-acute providers, such as home health and hospice agencies, have experienced difficulties in keeping qualified staff and have been more limited in providing services.
One service area that thus far has not experienced a significant decline in census is PACE. PACE programs provide services in a PACE center, which is similar to an adult day center but includes a clinic and also provides services within the participant’s home. Because of COVID-19, PACE centers have largely been limited to providing only clinic services over the past few months; however, expanded use of telehealth services has allowed the programs to closely monitor participants’ needs while minimizing physical contact.
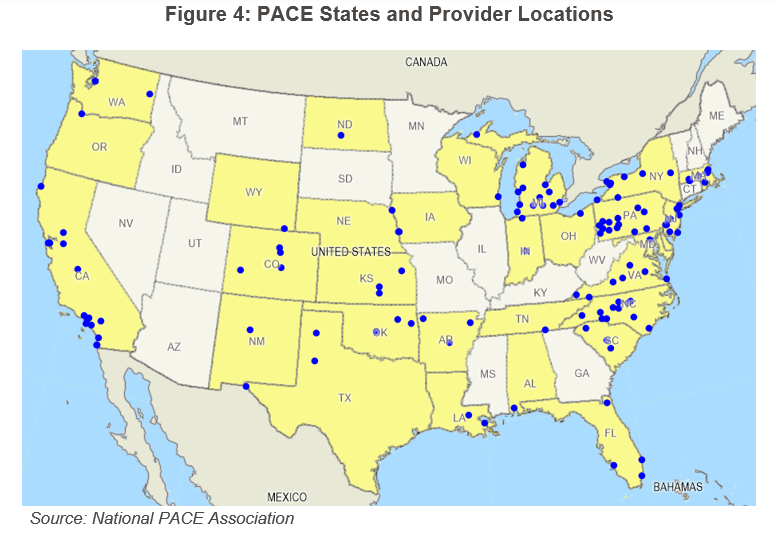
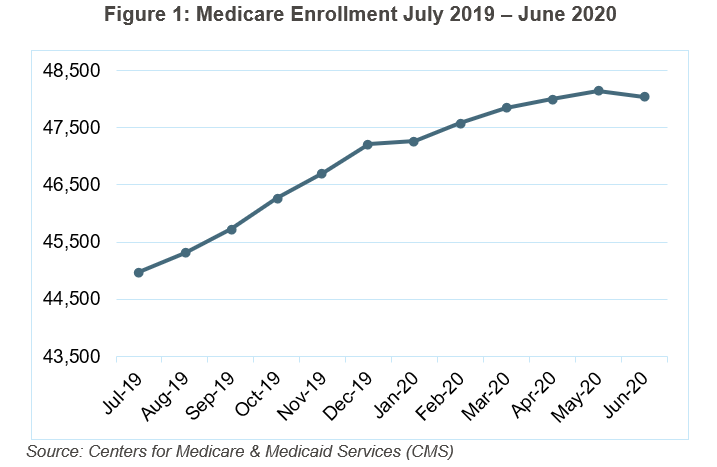
Medicare enrollment statistics for the past year (July 2019 to June 2020), are provided in Figures 1–3, below.
Dually-eligible individuals who are enrolled into both Medicare and Medicaid account for 90 percent of PACE enrollees. The remaining enrollees are either Medicaid only (9 percent) or “other” payers (1 percent), which typically include veteran contracts, long-term care insurance or private pay. The dually-eligible population increased from 44,978 participants in June 2019 to a peak of 48,133 participants in May 2020, with an overall increase in enrollment each month. June 2020 (48,040 participants) was the first time during COVID-19 that the national enrollment declined from the previous month.
The chart in Figure 2, above, shows the growth (percentage) from month to month. During COVID-19, growth was slower than in prior months, but still showed a minimal increase each month until June, which declined by 0.2 percent.
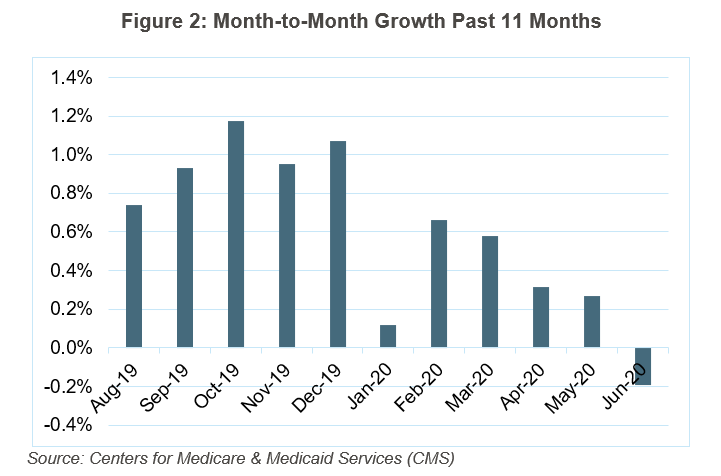
Although PACE enrollment has increased, not all programs have experienced the same changes. From July 2019 to June 2020, 34 programs have experienced a loss in dual-eligible participants, 2 programs have not changed, and 88 programs increased in dual-eligible participants. If we focus on calendar year 2020, we see 54 programs have declined in dual-eligible participants, 2 remained the same, and 74 have increased in dual-eligible participants.
It should be noted that although there are programs which have experienced either large increases or decreases, the median decline is 6 losses, while the median increase is 12 gains in CY20.
How Has PACE Not Been as Impacted as Other Senior Services Providers?
PACE is an at-risk model, which means the program is responsible for the care of its participants. Unlike traditional Medicare Fee-for-Service (MFFS), PACE programs have flexibility in how capitation dollars are used to provide the services their participants need. With PACE centers being closed or limited to only necessary clinic visits, programs have had to be creative in developing new ways to care for participants. These creative measures include redefining staff responsibilities, utilizing telehealth technology, and shifting to delivering care and meals in the home rather than in the PACE center.
If there is a silver lining for PACE programs during this pandemic, it is that the ingenuity displayed by PACE leaders may reveal new approaches to the PACE model of care that will continue to evolve after the COVID-19 pandemic runs its course.
Future Growth of PACE
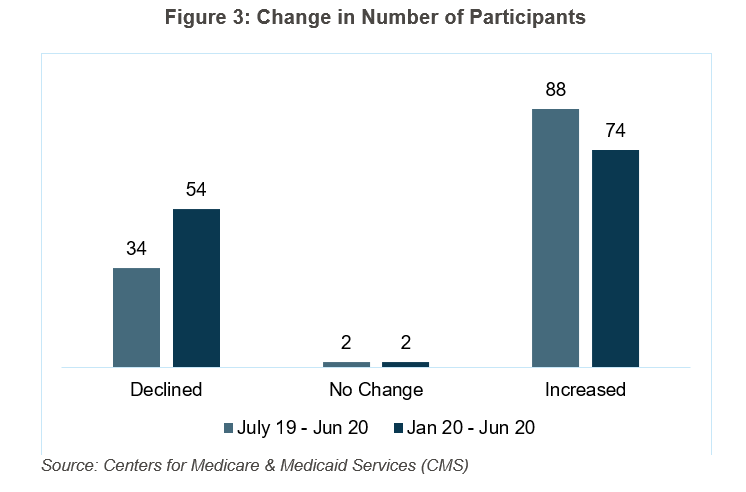
Starting a program generally takes 18–24 months. Even though COVID-19 has delayed PACE development in some states, two new programs have opened in 2020.
COVID-19 has highlighted the capabilities of the PACE model, and interest from organizations and financial investors in sponsoring PACE has accelerated, which is an indication that significant growth in new PACE plans is coming within the next few years.
For More Information
As a National PACE Association Technical Assistance Center, Health Dimensions Group (HDG) has successfully assisted many organizations with PACE market and financial feasibility studies, program development and implementation support, and operational improvement. If you would like to learn more about how HDG can assist you in exploring PACE as a solution in today’s challenging health care environment, please call or email us at 763.537.5700 or info@hdgi1.com and visit our website.