
The Centers for Medicare & Medicaid Services (CMS) published a proposed rule for Medicare payments to skilled nursing facilities (SNFs) for FY 2022 early this year. Along with the usual topics mentioned every year, the proposed rule packed a punch with a proposed 5 percent downward adjustment to payment rates to maintain budget neutrality. The only good news is that CMS is proposing to apply this adjustment prospectively once finalized. The potential impact of this “recalibration of the parity adjustment,” as well as the reasons behind it, have important implications for skilled nursing providers.
Background
When CMS implemented the Patient-Driven Payment Model (PDPM) on October 1, 2019, the agency made it clear the new system was intended to be budget neutral. The federal government essentially defined budget neutrality as what Medicare would otherwise have paid if the previous payment system, Resource Utilization Groups – Version 4 (RUG-IV), had still been in place.
This definition of budget neutrality poses several challenges for CMS, which it readily acknowledges:
- The COVID-19 pandemic created an entirely new patient population that did not exist under the RUG-IV system. In 2020, it turns out that approximately 10 percent of SNF stays had COVID-19 as a primary or secondary diagnosis.
- Moreover, the implementation of the waiver of the three-day prior hospitalization requirement for SNF coverage may mean that utilization patterns could well have changed in a way that altered payments. In prior years, 98 percent of SNF stays had a qualifying prior hospitalization. Under the three-day prior stay waiver, 87 percent of SNF stays had a qualifying prior hospitalization—an 11-percentage point drop.
So, CMS created a database that factored those two issues out. Then they proceeded to compare PDPM to the previous payment system, RUG-IV. The basic challenge here is that these are two very different payment systems with different incentives. RUG-IV directly tied revenues to the provision of therapy, thus creating a financial incentive to provide therapy. PDPM undid that linkage—therein lies one of the rubs.
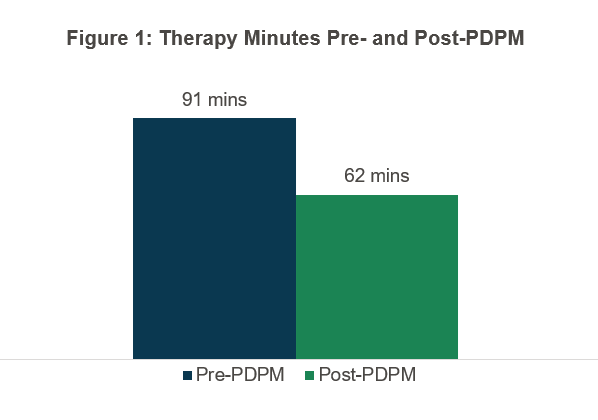
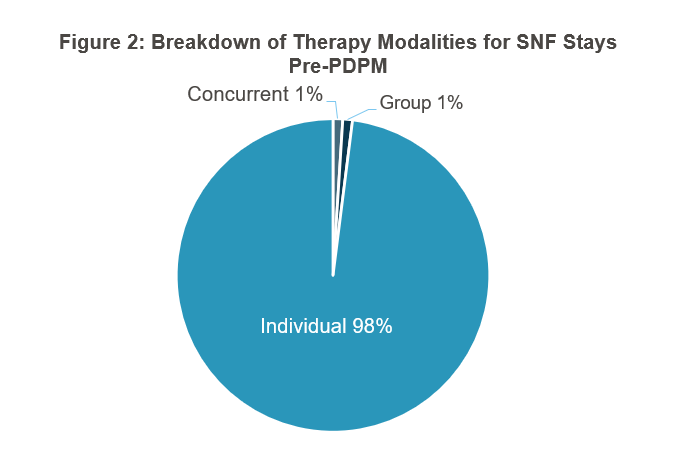
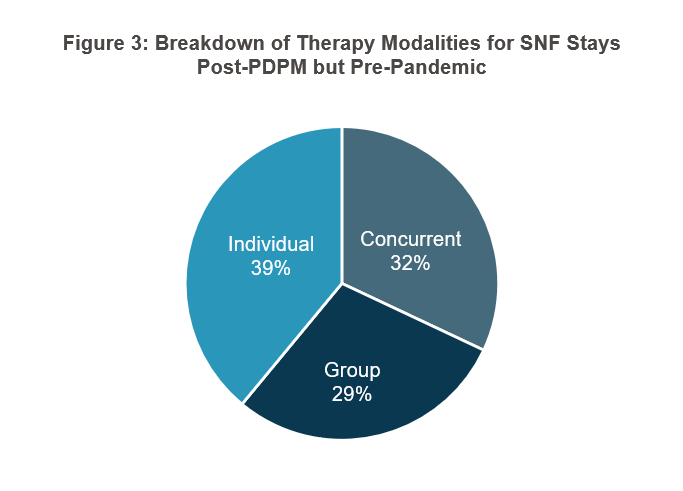
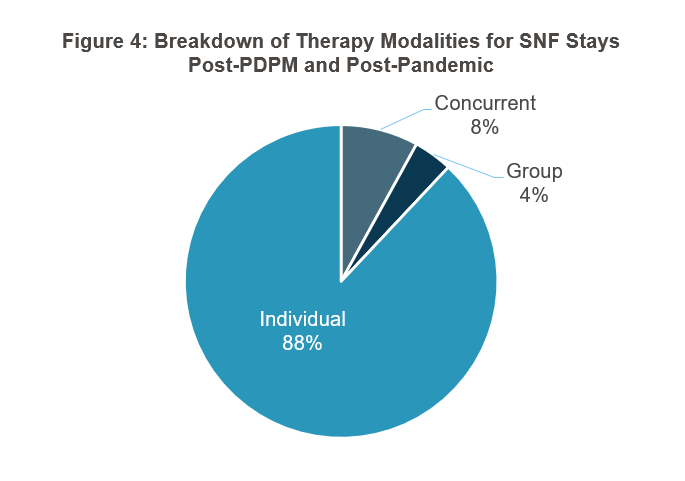
The data CMS provided on how therapy changed was both striking and not terribly surprising. Prior to PDPM, the average minutes of therapy was 91 minutes per day. As shown in Figure 1, it went to 62 minutes a day under PDPM—a 30 percent drop that CMS described as “immediate and ubiquitous.” CMS also shared some changes in group and concurrent therapy, going from 1 percent of stays for each pre-PDPM to 29 and 32 percent respectively until the pandemic hit, whereupon they settled at 4 and 8 percent, respectively (see Figures 2–4). Interestingly, CMS cites several quality metrics that indicate to the agency that patient outcomes did not suffer despite the large drop in therapy minutes.
 These changes in therapy mean that if PDPM payments were to be compared to what payments would have been under RUG-IV, a serious payment cut would have been necessary to keep payments budget neutral. Recognizing this, CMS then proposed to calculate the RUG-IV payments for comparison purposes based on the immediate prior year’s RUG distribution and then compare it to PDPM, after adjusting for payment updates.
These changes in therapy mean that if PDPM payments were to be compared to what payments would have been under RUG-IV, a serious payment cut would have been necessary to keep payments budget neutral. Recognizing this, CMS then proposed to calculate the RUG-IV payments for comparison purposes based on the immediate prior year’s RUG distribution and then compare it to PDPM, after adjusting for payment updates.
In doing the PDPM part of that calculation, CMS provides a chart that should be of interest to all SNF providers. The chart shows case mix indices by PDPM component for what was originally projected under PDPM compared to what actually happened in 2020.
Table 1: Case Mix Indices for PDPM Components – Projected Compared to Actual
| PDPM Component | FY 2019 – Estimated | FY 2020 – Actual | FY 2020 – Actual Less COVID and Waiver | Percent Change – Adjusted Actual Over Estimated |
| Physical Therapy | 1.53 | 1.50 | 1.52 | -1% |
| Occupational Therapy | 1.52 | 1.51 | 1.52 | 0% |
| Speech Language Pathology | 1.39 | 1.71 | 1.68 | 21% |
| Nursing | 1.43 | 1.67 | 1.62 | 13% |
| Non-Therapy Ancillary | 1.14 | 1.20 | 1.21 | 6% |
Source: CMS proposed rule SNF PPS, April 8, 2021
Health Dimensions Group (HDG) is not surprised at these figures, as we have been benchmarking SNFs over the last year. Of note is the 21 percent increase in Speech Language Pathology case mix index, as well as the 13 percent increase in Nursing and 6 percent increase in Non-Therapy Ancillary case mix indices. The policy questions raised by this table are whether the increases in case mix indices resulted from changes in facility practices in response to PDPM or were simply the result of more attention to coding (or both). This has been an age-old question in new case mix systems and surely will be a topic for comments to CMS.
Implications for SNF Providers
There are four main implications for SNFs:
- First, the proposed rule is in a comment period ending June 9, 2021. Providers with issues in the CMS proposal should make their views clear. The proposed rule can be found here.
- Second, therapy contracts signed just before PDPM started that have not been recently reviewed should be carefully assessed before being renewed. If the contract pays the therapy provider a percentage of the PDPM rate or percentage of therapy component, providers should make sure that the parameters of the contract comport with current market norms. Therapy contracts should be moving to a value-based component by having quality metrics directly incorporated into the payment structure to ensure that quality is not sacrificed for cost savings.
- Third, PDPM case mix indices should be benchmarked against emerging market norms to ensure that facilities are capturing all that they are entitled to. This benchmarking must be done in an apples-to-apples fashion. The proposed 5 percent rate hit, if enacted, will essentially charge each facility as if it upcoded at the nationwide average rate, whether it did so or not.
- SNFs should strongly consider making what we call the “medical complexity pivot.” PDPM provides dynamic adjustment to the rates for facilities taking higher acuity patients, such as those requiring dialysis, respiratory care, and total parenteral nutrition. In a post-pandemic world, it will be critical for facilities to increase their clinical capabilities and reach out to health systems and payors to make sure they are addressing their needs.
Facing the Future
Health Dimensions Group is ready to assist providers in responding to PDPM to thrive in a post-pandemic world. Our consulting experience is informed by our real-world work as operators. Please contact us at 763.537.5700 or info@hdgi1.com and visit our website to learn more about how we can help you prepare for a brighter future.





