Individuals with multiple chronic conditions and advanced illness place a distinct burden on the United States health care system, representing but 5 percent of the population while consuming upwards of 50 percent of the resources. To achieve person-centered outcomes at a competitive cost profile, these individuals require an integrated, coordinated continuum of care that includes traditional health care services as well as psycho-social support services.
Unfortunately, the continuum of health care and psycho-social support services most often is fragmented and under the purview of different agencies and professionals. These components, whether based in the home, community, or an outpatient or institutional setting, work in parallel with separate funding streams and budgets; under disparate and frequently conflicting regulations; and with different roles, responsibilities, and “languages” spoken.
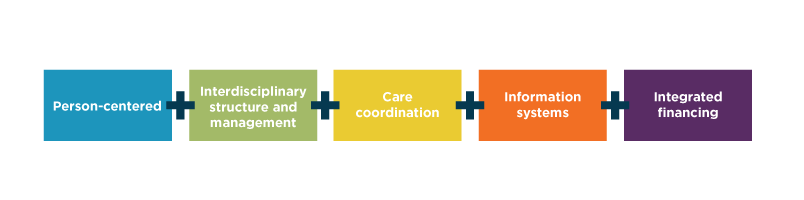
In response, there has been significant growth in integrated options for persons living with frailty, multiple chronic conditions, and advanced illness. These integrated options require five pillars to be successful.
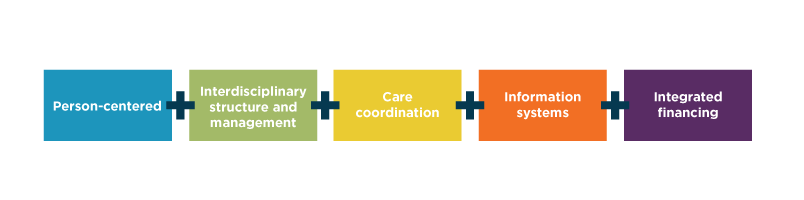 These pillars create boundary-spanning mechanisms that ensure “horizontal” integration across services and “vertical” integration across structures and financing. Most important, these pillars result in a person-centered model of care that moves the focus to patient and family needs—not to the toolbox of services available to be delivered.
These pillars create boundary-spanning mechanisms that ensure “horizontal” integration across services and “vertical” integration across structures and financing. Most important, these pillars result in a person-centered model of care that moves the focus to patient and family needs—not to the toolbox of services available to be delivered.
The Program of All-inclusive Care for the Elderly (PACE) is considered the “gold standard” of integrated, comprehensive person-centered care. PACE addresses the medical, social, and personal needs of frail, community-residing older adults. Organized to maximize the health care and social advantages of an adult day center, an interdisciplinary team of PACE professionals strives to holistically meet these needs to enable participants to live and thrive in their community, maintaining independence as long as possible. Financing is a partnership of Medicare and state Medicaid. The person-centered, interdisciplinary team-based care and integrated financing explains, in large part, the efficiency and exceptional quality outcomes associated with the model.
This track record of success, together with recent developments such as new opportunities for regulatory and enrollment flexibility; faster time to market with a more efficient application process; and the recent option for previously discouraged for-profit program sponsorship, has created much deserved interest in PACE. These developments, among others, indicate the Centers for Medicare and Medicaid Services believes in the financial and clinical outcomes of PACE and is encouraging faster growth and expansion.
ACOs, health systems, managed care organizations, and senior living communities are increasingly recognizing the symbiotic relationships possible with PACE, when viewed as a key population health management tool for select segments of medically complex individuals. This has driven many to look to PACE sponsorship as a key component of their population health strategy.
As a PACE Technical Assistance Center and leading post-acute and senior care management and consulting firm, Health Dimensions Group is recognized as a leader in PACE consulting. In celebration of National PACE Month, please join us for a PACE programming webinar on Wednesday, September 13, from noon to 12:30 p.m. Central Time. HDG will provide an overview of the PACE model and the assessment process for understanding how a PACE program could be a key success driver in your population health strategy.

