
On September 1, 2023, the Centers for Medicare & Medicaid Services (CMS) released a highly anticipated proposed rule entitled “Minimum Staffing Standards for Long-Term Care Facilities and Medicaid Institutional Payment Transparency Reporting.” The proposed rule was 18 months in the making as part of a broader set of nursing home reforms released by the White House back in February 2022.
Comments on the proposed rule are due November 6, 2023. This will provide all stakeholders with an opportunity to have their voices heard. Ideally, this process will result in a meaningful conversation about how to truly drive quality in nursing homes and adequately fund it.
BASICS OF THE MINIMUM STAFFING STANDARDS PROPOSED RULE
The rule has “three core staffing proposals: 1) minimum nurse staffing standards of 0.55 hours per resident day (HPRD) for Registered Nurses (RNs) and 2.45 HPRD for Nurse Aides (NAs); 2) a requirement to have an RN onsite 24 hours a day, seven days a week; and 3) enhanced facility assessment requirements.”[1]
These proposed minimums would be implemented in a phased-in manner over a period of two to five years from finalization (except for the facility assessment requirements, which will go into effect within 60 days of finalization). There will be the possibility of hardship exemptions based on geographic proximity to other facilities or workforce shortage. The proposed rule also contains a transparency component based on the percentage of Medicaid payments for services in nursing homes that are spent on compensation to direct care workers and support staff. Finally, CMS has included over $75 million in financial incentives, such as scholarships and tuition reimbursement, to help make it easier to enter the long-term care (LTC) workforce.
SHRINKING WORKFORCE RELATIVE TO DEMAND
One of the biggest concerns raised by the proposed staffing minimums is whether a sufficient workforce will be present when those requirements go into effect between two and five years from now.
Health Dimensions Group (HDG) routinely conducts market analysis for our clients in which we dissect a market from both an elderly and workforce demographics perspective. The challenges that lie before us are clear: double-digit projected growth in the elderly population compared to flat or minimal growth in the workforce population.
The following chart from the Medicare Payment Advisory Commission (MedPAC) illustrates the problem by showing that the number of available workers per Medicare beneficiary has been on a steady decline and is going to continue to decline over the next five years.
Figure 1: Workers Per Medicare Beneficiaries
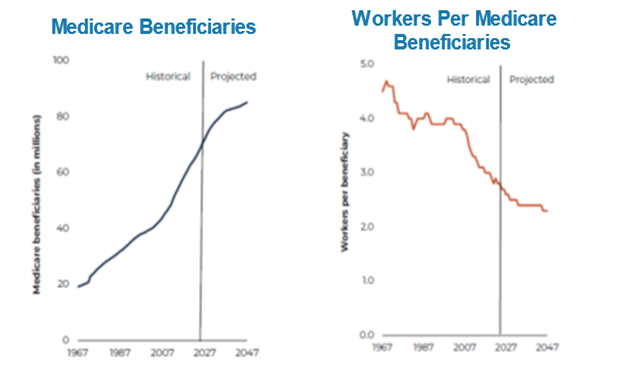
Source: MedPAC.
In the context of the proposed rule, this means several things.
For one, current workforce shortages have the likelihood of being even worse when the staffing minimums go into effect. It is not at all clear that the proposed hardship exemptions will be sufficiently helpful to address widespread workforce supply problems.
Second, the projected real growth in wages (net of inflation) created by these mandates is likely to be much higher than the 2.3 percent annual growth that CMS used to project costs in the proposed rule. The 2.3 percent figure was derived from data from staffing mandates implemented years ago and reflected a very different labor market than today’s environment. The 2.3 percent real wage growth assumption needs to be revisited by conducting more sophisticated economic modeling.
More important, it seems clear that strategies to increase the supply of nurses should be given the highest priority. The $75 million incentive fund for scholarships and tuition reimbursement is likely to be a drop in the bucket compared to what is really needed.
LACK OF THIRD-PARTY FUNDING
The proposed rule does not contain a mandate for Medicare and Medicaid to adjust their rates in consideration of these new proposed staffing mandates. This is especially important with respect to Medicaid, which pays for the majority of residents in nursing homes. The rule contains a proposed transparency requirement to collect and post the percentage of Medicaid payments for services in nursing homes that are spent on compensation to direct care workers and support staff. Ultimately, this is yet another reporting requirement that does not directly lead to an assessment of how much additional funding is actually needed, nor does it ensure that those funds will be made available.
TIME TO RETHINK INCENTIVIZING QUALITY
Many states have quality incentive programs as part of Medicaid payments to nursing homes. These programs are highly variable in their scope, quality metrics utilized, and perceived effectiveness. Now is a good time to re-evaluate Medicaid quality incentive programs and restructure them to address resource-intensive initiatives—such as 24/7 RN coverage—in an incentive framework that provides additional funding as necessary. Another important timing element is that many state Medicaid programs are making the transition from a RUGs-based payment system to a version of the Patient-Driven Payment Model (PDPM). This is an opportunity to enhance the ability of Medicaid payment reform to support quality.
Although staffing is an important aspect of quality of care, there are other resource-intensive issues that should also be considered in a quality reform agenda, including upgrading the physical plant, implementing interoperable technology, and increased training. The federal government could aid in the process of reforming Medicaid quality incentive programs by convening the states, issuing guidelines, and providing additional funding for simple, clear, and direct incentives incorporated into Medicaid payment rates.
WHAT HAPPENED TO LPNS?
Regardless of what the federally funded Abt study showed about the impact of licensed practical nurse (LPN) staffing on quality, LPNs are a vital part of most nursing homes. Unfortunately, the proposed staffing standards do not count LPNs. This could cause hardship in certain markets where RNs are very scarce and LPNs are relatively plentiful. Worse yet is the potential for the unintended consequence of minimizing the presence of LPNs because they “no longer count.” CMS really needs to rethink this one.
REVAMPING CARE PLANNING
Finally, to end on a positive note, it is our hope that the proposal to revamp care planning will spur a dialogue on this important topic. Specifically, the proposal to use evidence-based methods and develop a staffing plan should be fleshed out and consensus should be achieved about what that means and how to go about doing so. To be frank, in this market, any facility without a proactive staffing plan is headed for trouble, if not there already.
HOW WE CAN HELP
HDG has provided this analysis to help stakeholders in forming their comments regarding the proposed rule. Those comments are due by November 6, 2023. HDG can also help with workforce solutions, market research, and policy analysis to help the LTC sector survive and thrive in this increasingly challenging market. Please contact us at info@hdgi1.com or 763.537.5700 for more information.











