
Deficiencies, F-tags, and civil monetary penalties (CMPs) are all a daily risk for any skilled nursing facility (SNF) or assisted living (AL) community operator, but there are certainly trends to watch for when assessing your building’s clinical or operational regulatory risks. Over the last three years, total fines for just one SNF in Florida came in around $948,000; one SNF provider in Tennessee also tallied up about $935,000.[1] Among the most recent serious deficiencies (as of October 2023) were the following:
- Failure to provide and implement an infection prevention and control program.
- Failure to immediately tell the resident, the resident’s doctor, and a family member of situations (injury/decline/room, etc.) that affect the resident.
- Failure to ensure that a nursing home area is free from accident hazards and provides adequate supervision to prevent accidents.
With almost 30 percent of SNFs not receiving a recertification survey in more than 15 months (CASPER data captured between October 1, 2022, and September 30, 2023), the likelihood of an increase in citations resulting from these deficiencies is high.[2]
It should come as no surprise that two of the three deficiencies listed above were also the most cited during 2023. A search in the Quality, Certification and Oversight Reports (QCOR) system indicated the following five F-tags were cited the most over the last year:
- F0884: Reporting – National Healthcare Safety Network
- F0689: Free of Accident Hazards/Supervision/Devices
- F0880: Infection Prevention & Control
- F0812: Food Procurement, Store/Prepare/Serve – Sanitary
- F0684: Quality of Care
Figure 1: Top 5 F-tags in 2023
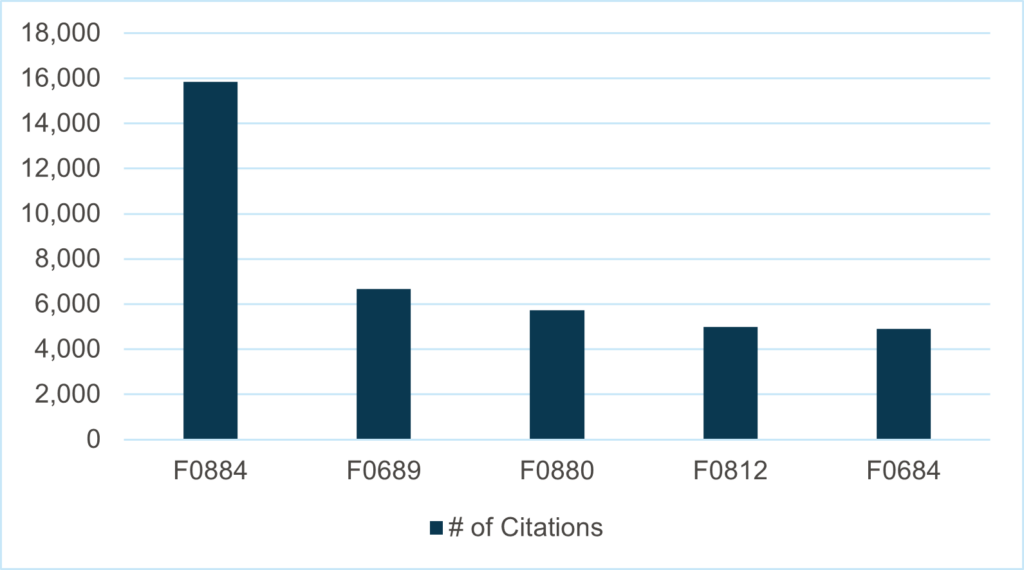
Source: Quality, Certification and Oversight Reports (QCOR), http://qcor.cms.gov/
While Health Dimensions Group (HDG) can help you address and correct potential deficiencies—including these five—there are a number of ways you can prepare for and tackle them before they have an effect on your star ratings or bank accounts.
Prepare for Your Next Survey by Tackling the Most Common Issues
F0884: Reporting – National Healthcare Safety Network
Given the continued presence of COVID-19, specifically in SNFs or senior living campuses, it is no wonder that the accurate and timely reporting of COVID-19 infections to the National Healthcare Safety Network (NHSN) stands as the most cited deficiency of 2023. As seen in Figure 1, the number of citations for F0884 far exceeds all others.
This citation is the lack of COVID-19 reporting to the Centers for Disease Control and Prevention (CDC). F0884 is the only regulation in the nursing home Requirements of Participation (ROP) that is not surveyed by state surveyors and should not be cited as an F-tag. Instead, Centers for Medicare & Medicaid Services (CMS) federal surveyors will complete an off-site review and identify facilities that are not reporting and issue a deficiency citation with a scope and severity level at an F to an immediate jeopardy (IJ).
Facilities can help themselves maintain compliance by continuing to report COVID-19 data to state and local health departments. The NHSN is not a replacement for state and local public health reporting requirements. The best practice—whether your facility is a stand-alone or part of a larger corporation—is to establish one person (along with a trained backup) to be responsible for the weekly report to CMS.
F0689: Free of Accident Hazards/Supervision/Devices
According to the CMS State Operations Manual, Appendix PP (Guidance to Surveyors for Long Term Care Facilities), “the facility must ensure that…the resident environment remains as free of accident hazards as is possible; and…each resident receives adequate supervision and assistance devices to prevent accidents.”[3] The intent of this requirement is for facilities to provide an environment free from accident hazards that the facility can control and provide supervision and assistive devices to prevent avoidable accidents, such as a fall with injury with a failure to follow the care plan interventions or an added intervention to prevent the incident from occurring again. Therefore, it is necessary for facilities to do the following:
- Identify hazards and risk
- Evaluate and analyze hazards and risk
- Implement interventions to reduce hazards and risk
- Monitor effectiveness and modify if needed
To maintain compliance, facilities should have a robust risk management program that is reviewed daily in the morning meeting with follow-up of intervention in an afternoon meeting. It is necessary to identify and eliminate or reduce the risk of all known and unexpected accident hazards in the resident’s surroundings. Appropriate and sufficient supervision and assistive devices necessary to prevent avoidable accidents must be provided. Facilities need to complete an accident supervision investigation summary for each incident that includes interviews of all staff and others in the immediate area of the accident. Most of all, document, document, document!
F0880: Infection Prevention & Control
Without a doubt, COVID-19 outbreaks have become what first comes to mind when one sees an F0880 tag; however, many citations have applied to oversights such as handwashing or proper personal protective equipment (PPE) usage.2
Long-term care facilities must develop and implement an ongoing infection prevention and control program (IPCP) to prevent, recognize, and control the onset and spread of infection to the extent possible and review and update the IPCP annually and as necessary. This includes revision of the IPCP as national standards change.[4] The intent is to establish a facility-wide system that allows residents, staff, and visitors to remain free of infections and communicable diseases, including following national standards for handwashing, linens and laundry handling, storing, processing, and transporting by staff to prevent infection. Written policies and procedures for infection control must be developed and implemented, and can include the following:
- Resident care activities should include explanation of standard precautions to prevent the spread of infection.
- How and when to utilize transmission-based precautions, including the type and duration of precautions.
- Staff with communicable disease or infected skin lesion are restricted from direct contact with residents or their food.
- Hand hygiene practices must be consistently followed by staff.
In order to maintain compliance, a facility should develop an IPCP that provides a safe, sanitary, and comfortable environment, with a focus on preventing disease and infection. Even though it falls under another F-tag, it is important to have a trained infection preventionist (IP) that oversees the IPCP and a trained backup for times the IP is out. A system must be maintained for recording incidents and taking appropriate corrective actions.
F0812: Food Procurement, Store/Prepare/Serve – Sanitary
No matter the year, F0812 regularly makes it to the top of the list as one of the most cited regulations. There are many areas of concern when it comes to food preparation and sanitation for SNFs and senior living communities: poor personal hygiene, improper cooking and serving temperatures, contaminated equipment, and unsafe food sources.3
Facilities must obtain food for resident consumption from sources approved by federal, state, or local authorities. That food must be stored, prepared, distributed, and served in accordance with professional standards. Facilities must follow proper sanitation procedures and food handling practices to prevent outbreak of foodborne illness. When serving buffet-style food from a steam table or during a potluck, food safety must be maintained by the facility.
A facility will remain in compliance by maintaining food safety, including procuring, storing, handling, preparing, distributing, and serving food in the following ways:
- Staff should maintain food at safe temperatures, for hot/cold, during preparation, cooking/cooling, and food plated for transport.
- Raw foods should be stored in a manner to avoid contamination of other foods.
- Food should be cooked to appropriate temperatures to kill pathogenic microorganisms that may cause foodborne illnesses.
- Food should be cooled in a way to avoid growth of pathogenic microorganisms.
- Staff must use proper hand hygiene and should be monitored for such practice.
- Kitchen equipment should be maintained, clean, and free of food particles to prevent cross-contamination.
It is best practice for the facility dietitian to complete a monthly sanitation audit and have the dietary manager complete a quality assurance and performance improvement (QAPI) plan to correct all issues identified. It is also important to ensure that food service employees have received training related to compliance with food service documentation, policies and procedures, food sanitation and safety, monitoring records such as temperature log for tray line, refrigerator and freezers, dishwashers and sanitizing. Remember to watch your eggs—sunny-side up, soft scrambled, and soft boiled—to make sure you are using pasteurized shell eggs or liquid pasteurized eggs.
F0684: Quality of Care
This F-tag is centered around ensuring nursing home residents are receiving the required treatment based on their individual personal care plan. Deficiencies are most often cited if staff does not notify the resident’s physician of a change in their medical needs or condition, or if there is a failure to provide needed care or services that results in a decline or potential decline in a resident’s overall well-being.
Often considered a “catch-all” citation, it applies to all treatment and care provided to facility residents. Facilities must be able to ensure and identify that residents receive treatment and care in accordance with professional standards of practice. Facilities must also provide needed care and services that cater to each resident’s preferences and meet their physical, mental, and psychosocial needs.
In order to cite facilities under this citation, surveyors will look for evidence that the facility failed to provide care and services that resulted in an actual or potential decline in a resident. Surveyors also look for factors that place residents at risk for a specific condition. It is important to monitor residents’ responses to interventions that are ineffective or place residents at further risk. Ensure that your facility is developing a resident-directed care plan with a comprehensive assessment and input from resident and resident representative on preferences, choices, and goals. Most importantly, inform and educate residents who choose to refuse or decline care about the “risk versus benefits” of doing so. Remember, it is important to offer residents choices or other options to minimize further decline or negative outcomes. Finally, document, document, document!
Conclusion
These deficiencies are all avoidable if the proper education and processes are established for your facility, which will result in improved care, better CMS star ratings, and lower CMPs. With today’s challenges—declines in SNF bed occupancy, upcoming federal nursing home mandates, and staffing shortages—facilities cannot afford to compound these issues with improper care for residents or additional financial burdens.
If you find yourself struggling to maintain regulatory compliance or establish policies and procedures to improve your current situation, please reach out to HDG for a Positive Review and Evaluation Process (PREP) mock survey, in which a wide range of activities—including nursing, recreation and activities, staffing, administration, dietary and meal service, abuse prevention, medication administration management, infection prevention and control, QAPI, life safety code, and emergency preparedness—are assessed in order to help reduce your facility’s risk for deficiencies. To learn more, please contact us at info@hdgi1.com or 763.537.5700.
[1] ProPublica, Nursing Home Inspect, https://projects.propublica.org/nursing-homes/
[2] McKnight’s Long-Term Care News, Standard Surveys Continue to Lag, with Infection Control a Major Tripwire, https://www.mcknights.com/news/standard-surveys-continue-to-lag-with-infection-control-a-major-tripwire/
[3] CMS State Operations Manual, Appendix PP, https://www.cms.gov/medicare/provider-enrollment-and-certification/guidanceforlawsandregulations/downloads/appendix-pp-state-operations-manual.pdf
[4] American Health Care Association, The Long Term Care Survey, Phase 3







