
Growth of the Program of All-Inclusive Care for the Elderly (PACE) remains strong in 2023 and does not seem to be slowing down from the momentum of the past couple of years. Twenty-one programs have opened since 2020, and some estimates predict more than 40 new programs could open in the next few years.
PACE PHILOSOPHY AND NEW 2023 PROGRAMS
PACE centers on the belief that it is better for the well-being of seniors with chronic care needs, and their families, to be served in the community whenever possible. By providing or coordinating all needed medical and supportive services through an interdisciplinary team (IDT), PACE programs are able to provide the entire continuum of care and services to older adults with chronic care needs, while enabling them to maintain independence in their homes for as long as possible.
The number of new PACE providers grew by six programs in 2020, six in 2021, seven in 2022, and two so far in 2023. It typically takes approximately 18–24 months to start a program, so patience is required, and these programs all either opened during COVID-19 or began planning during COVID-19. As COVID-19 is further behind us, more program are opening as providers, payers, and states have seen the adaptability and benefits of PACE.
Figure 1 shows the number of current PACE providers by time frame of opening.
Figure 1: PACE Programs by Time Frame Opened
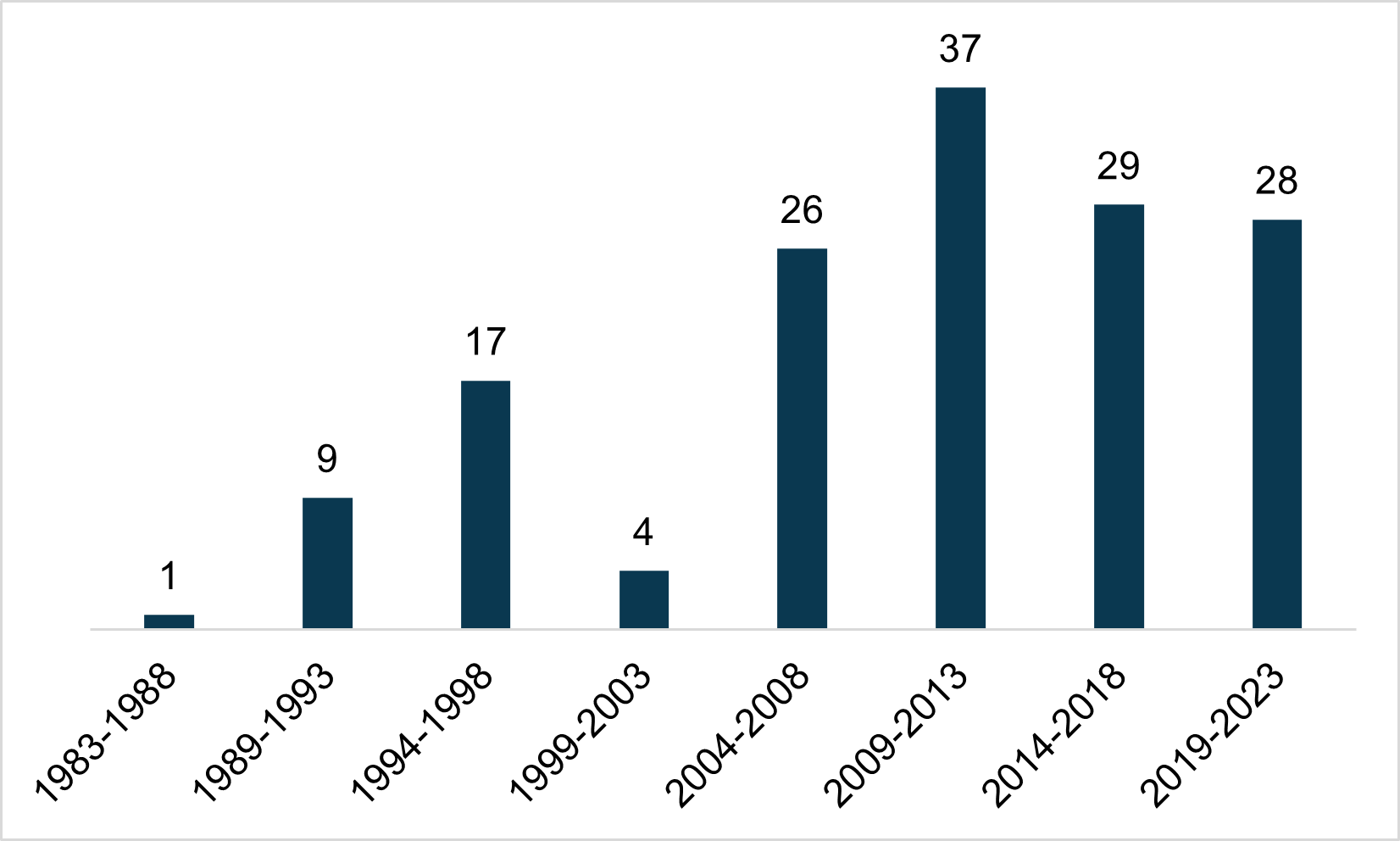
Source: National PACE Association (NPA)
Not including the first half of 2023, there were an average of six new PACE programs during the prior three years. Over the past 10 years, there has been an average of 6.3 new programs opened per year, putting the past few years near average, despite the expanded difficulties of opening during a pandemic. Two programs have opened in 2023 with six more months to go indicating the growth of new programs has remained stable.
DUAL-ELIGIBLE ENROLLMENT GROWTH
In order to be an candidate for enrollment into PACE, an individual must be:
- 55 years of age or older.
- Determined by the State Administering Agency (SAA) to require a level of care defined under the State Medicaid plan for coverage of long-term care services (i.e., clinically eligible for PACE).
- Residing in a specified PACE service area.
- Able to live in a community setting at the time of enrollment without jeopardizing his/her health or safety based on criteria set forth in the PACE program’s three-party program agreement.
Although income is not a criterion to enroll in PACE, approximately 99 percent of enrollees are Medicaid eligible, with about 90 percent being dually eligible for both Medicare and Medicaid. The remaining 1 percent is a mixture of alternative payment sources, such as private payment and VA contracts, who are then required to pay the Medicaid portion of the monthly capitation rate. Figure 2 summarizes the dual eligibles, who account for the highest portion of PACE enrollment.
Figure 2: Dual-Eligible PACE Enrollment in January 2022 – June 2023
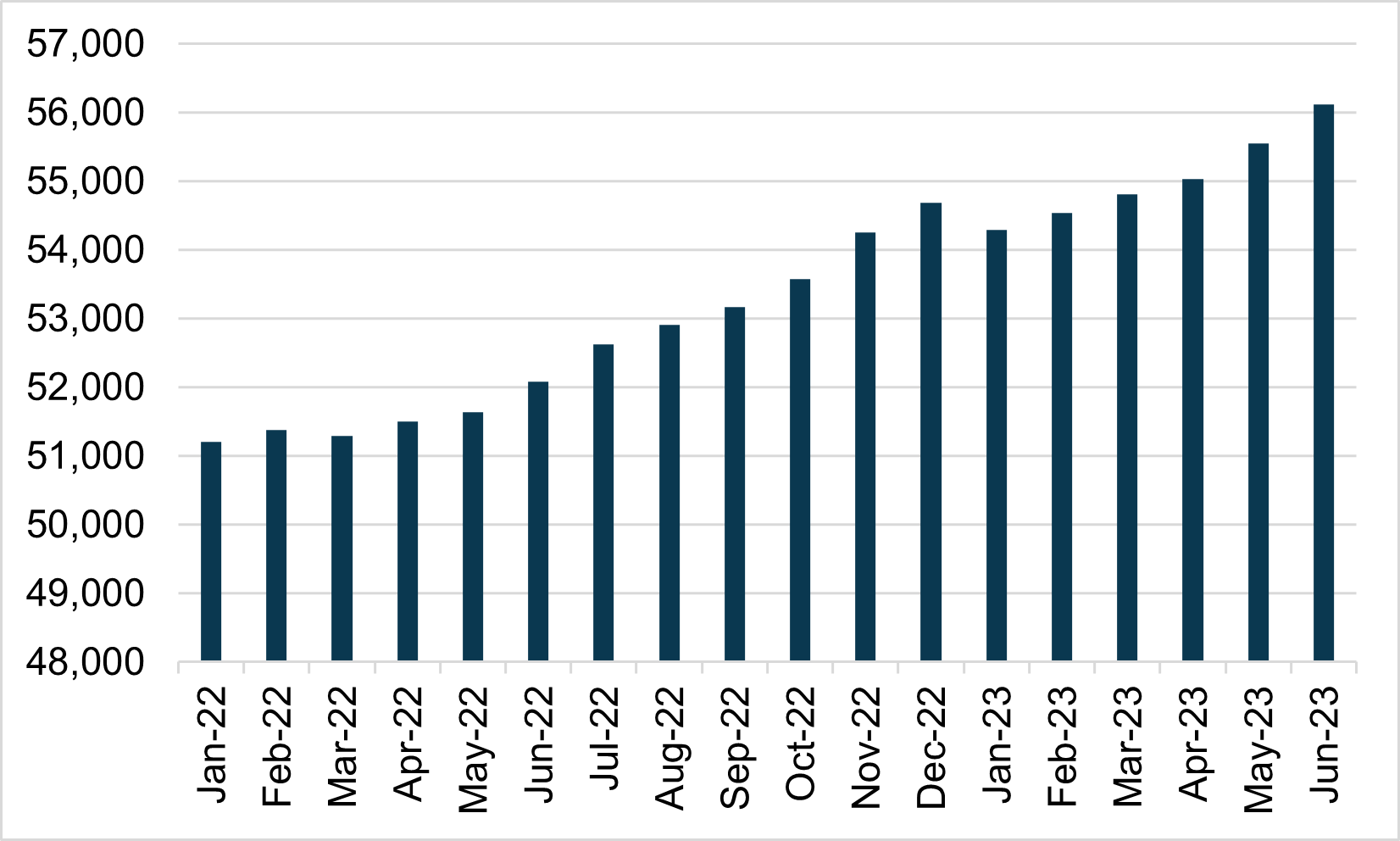
Source: Centers for Medicare & Medicaid Services (CMS)
With the exception of December 2022 to January 2023, national dual eligible enrollment in PACE increased every month since January 2022.
Some of the PACE dual-eligible enrollment growth is attributed to the addition of new programs. However, that only accounts for a small percentage of the overall increase. Figure 3 shows how the programs that were operational in January 2022 have fared since.
Figure 3: Dual-Eligible Enrollment Change in Programs Open All 18 Months
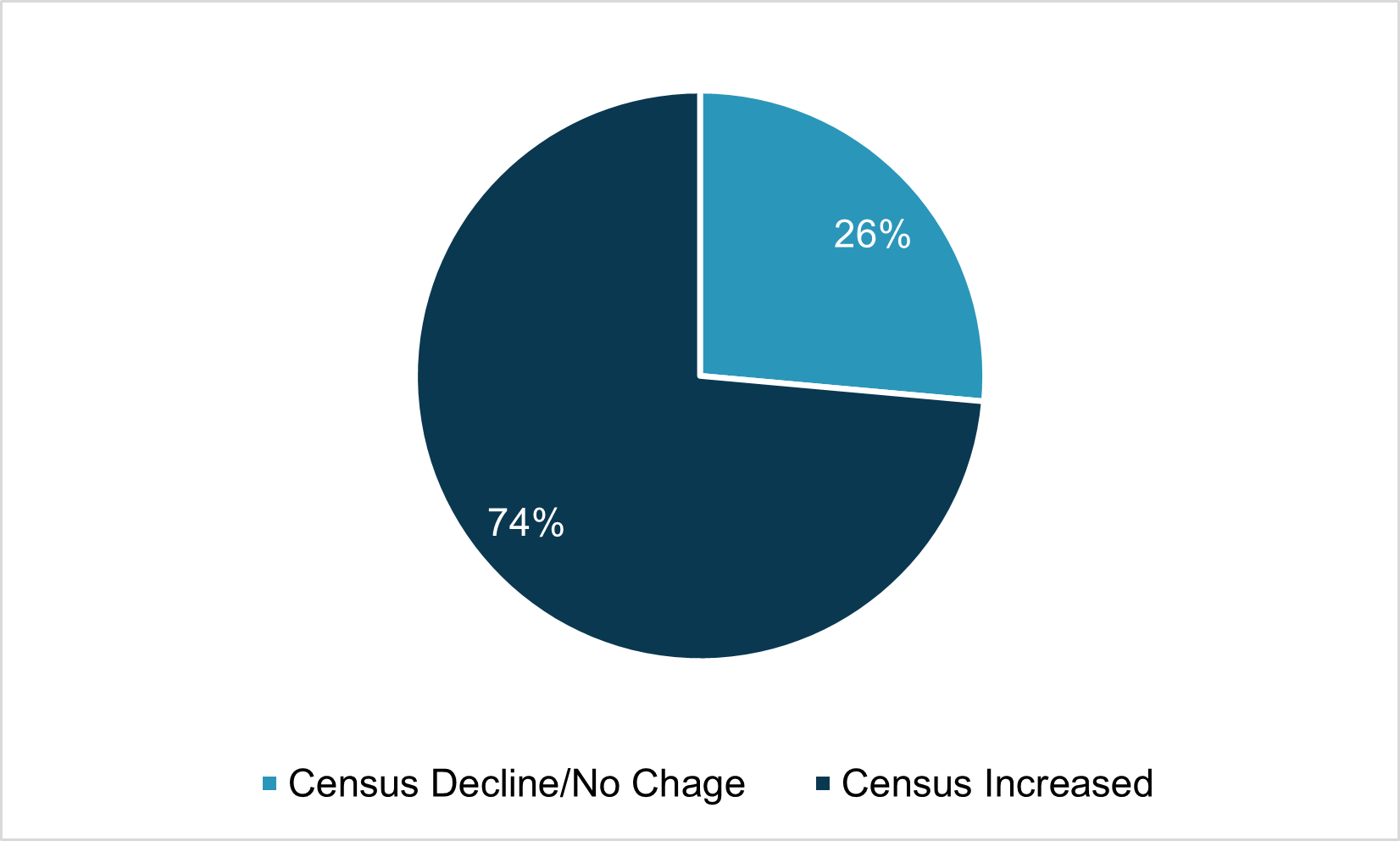
Source: CMS
As shown on Figure 3, for programs that were operating in January 2022, most have increased in census.
- Programs that experienced a decline in census or remained steady, the median decline was 13 enrollees.
- Programs that experienced an increase in census, the median increase was 34 enrollees.
- Overall, the programs that were open on January 1, 2022, experienced a cumulative growth of 8.9 percent through June 2023.
Figure 4 shows annual program growth for programs that were open for the full 12 months during prior years.
Figure 4: Annual Growth of Programs Open Full Year 2016–2023 (YTD)
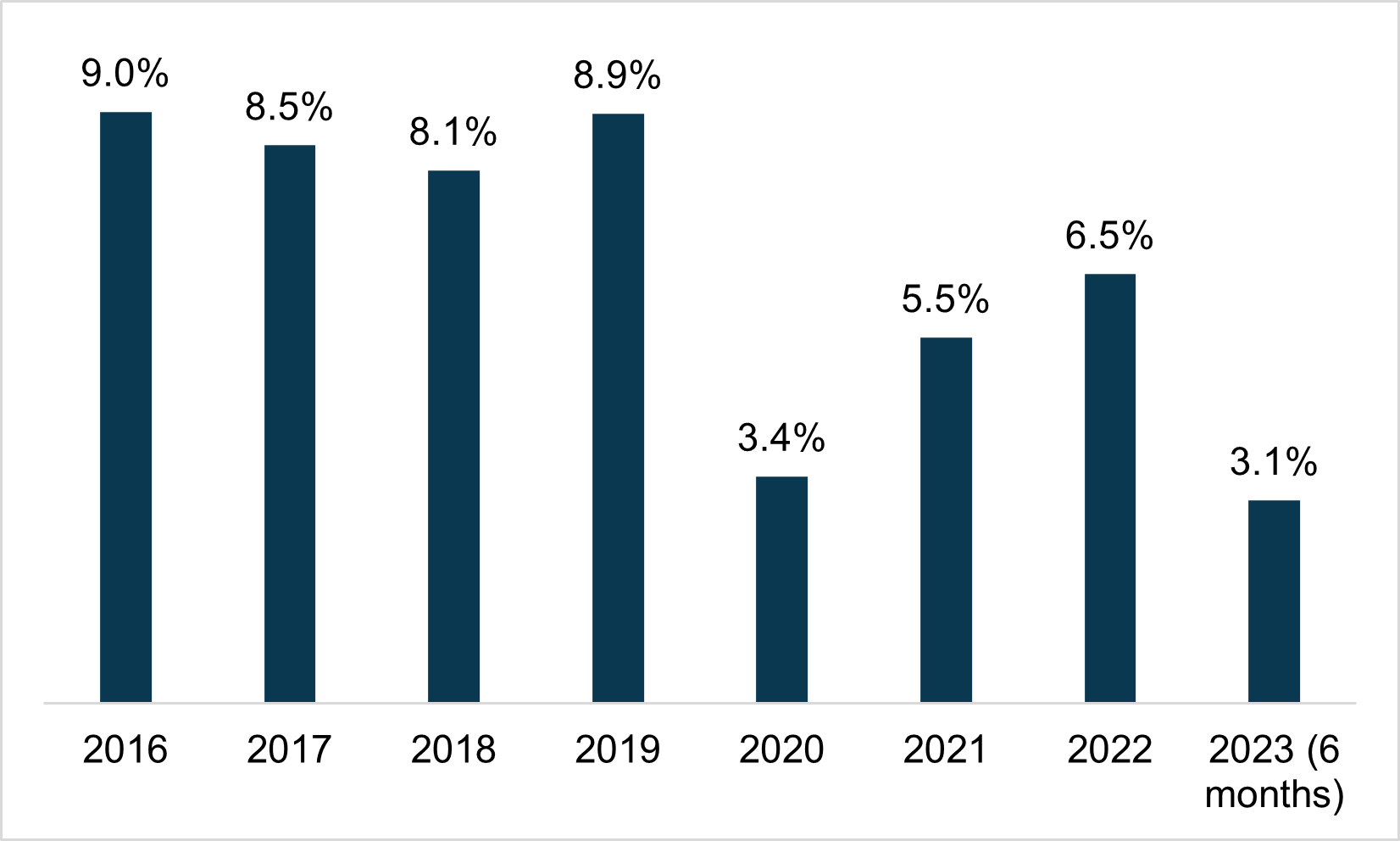
Source: CMS
As shown on Figure 4, if we eliminate any dual-eligible growth resulting from the opening of new programs, PACE programs experienced a cumulative annual growth of between 8.1 percent and 9.0 percent between 2016 and 2019. Although 2020 saw a significant decline in growth from prior years, PACE still experienced overall growth during the pandemic. Growth in 2021 and 2022 have not quite hit pre-COVID-19 levels but are higher than 2020. The first six months of 2023 has had nearly as much growth as all of 2020.
WHY DOES PACE CONTINUE TO GROW?
PACE is an at-risk model, which means the program is responsible for directly providing or coordinating and paying for all of its participants’ care needs. Unlike traditional Medicare Fee-for-Service (MFFS), PACE programs have flexibility in how capitation dollars are used to provide the services their participants need. When PACE centers were closed or limited to only necessary clinic visits, programs had to be creative in developing new ways to care for participants. These creative measures included redefining staff responsibilities, utilizing telehealth technology, and shifting to delivering care and meals in the home rather than in the PACE center.
If there is a silver lining for PACE programs during the pandemic, it was the ingenuity displayed by PACE leaders revealing new approaches to the PACE model of care that continue to evolve post COVID-19.
FUTURE GROWTH OF PACE
In response to the challenges of operating during COVID-19, many states encouraged the expansion of PACE. Existing PACE states such as Louisiana, Maryland, New Jersey, North Dakota, Ohio, Pennsylvania and Virginia released Requests for Proposals (RFP) for PACE expansion, while the District of Columbia and Illinois released RFPs to open their first providers. Kentucky and Missouri recently opened programs increasing the number of states to 32 that have an operational PACE program in addition to the District of Columbia. The increased federal funding for Medicaid home and community based services as part of the American Rescue Plan signed into law in March 2021 has caused many other states to consider investing in PACE development or expansion.
COVID-19 highlighted the capabilities of the PACE model, and interest from organizations and financial investors in sponsoring PACE has accelerated, which is an indication that significant growth in new PACE plans will continue for the foreseeable future. Figure 5 shows the number of programs operational as of June 2023.
Figure 5: PACE States and Provider Locations as of June 1, 2023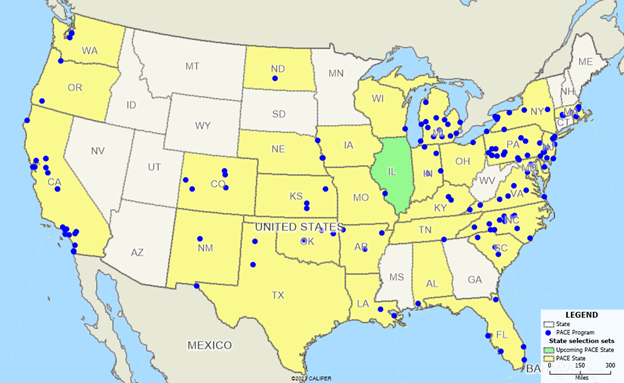
Source: National PACE Association
FOR MORE INFORMATION
As a National PACE Association Technical Assistance Center, Health Dimensions Group (HDG) has successfully assisted many organizations with PACE market and financial feasibility studies, program development and implementation support, and operational improvement. If you would like to learn more about how HDG can assist you in exploring PACE as a solution in today’s challenging health care environment, please contact us at 763.537.5700 or info@hdgi1.com.












